by Teresa C. Gallagher, Ph.D., MPH and and Martina Ambardjieva, M.D
For many men diagnosed with localized prostate cancer, the standard options, surgery or radiation, can come with tough choices. While these treatments can be effective, they often affect a man’s quality of life and urinary or sexual function. Understandably, one of the first questions men ask is:
“Are there alternatives that treat the cancer without taking such a big toll on my body?”
A growing number of urologists believe the answer may lie in focal therapy (FT) a treatment designed to target only the cancerous part of the prostate, while leaving the rest of the gland untouched. This approach aims to treat the disease effectively while preserving quality of life.
Focal therapy offers a middle ground for treating prostate cancer especially for men who want to avoid the life-changing side effects of surgery or radiation. It’s not a one-size-fits-all solution, but for well-selected patients with localized, intermediate-risk disease, it can be a powerful option that treats the cancer while preserving urinary and sexual function.
What Is Prostate Focal Therapy?
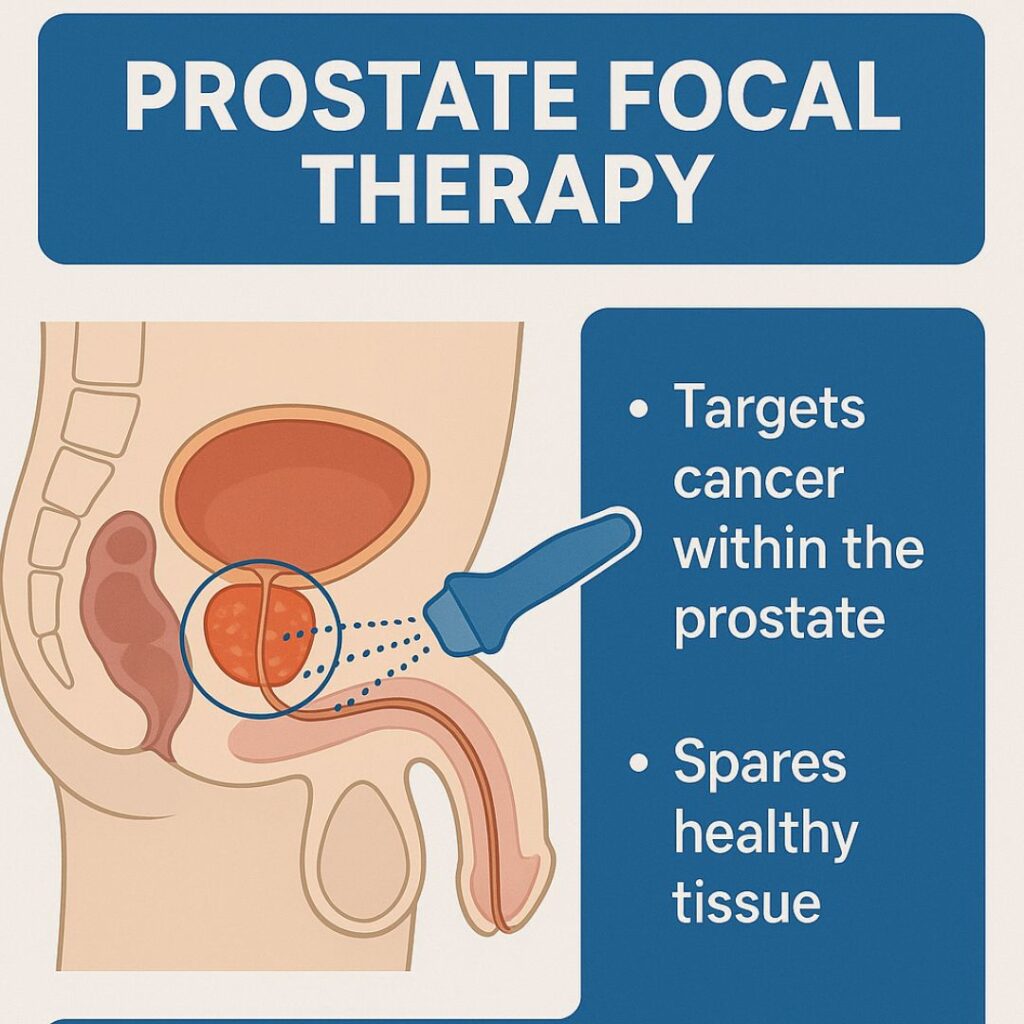
Prostate focal therapy is a minimally invasive approach that targets only the cancerous areas within the prostate gland. By preserving healthy tissue, it reduces the risk of side effects commonly associated with whole-gland treatments. This method is often considered for men with localized, low- to intermediate-risk prostate cancer.
Kinds Of Prostate Focal Therapy
According to the AUA (American Urological Association) there are several kinds of options for focal therapy:
1. Cryotherapy
Cryotherapy freezes the cancer using needles inserted into the prostate, often guided by MRI or ultrasound. It’s particularly useful for men with small, localized tumors. Studies show that failure-free survival at 3 years can reach 90%, especially in intermediate-risk patients. Most men maintain urinary continence, and about 84–86% preserve sexual function, though erectile dysfunction can occur. Cryotherapy is well tolerated and can be repeated if needed, though care must be taken to protect the urethra during treatment.
2. Focal Laser Ablation (FLA)
FLA uses laser energy to heat and destroy prostate tumors. It is often guided by MRI and offers real-time temperature control. While long-term data are still limited, early studies show that about 70% of men have no cancer in the treated area after 6–12 months, and urinary and sexual function is usually preserved. FLA is minimally invasive and can be performed in outpatient settings, but retreatment may be needed, and close follow-up with MRI and biopsy is important.
3. High-Intensity Focused Ultrasound (HIFU)
HIFU uses focused sound waves to heat and destroy cancerous tissue in the prostate. It’s performed using MRI or ultrasound guidance and targets just the tumor, sparing surrounding healthy tissue. In large studies, HIFU has shown high cancer control rates with up to 88% of men avoiding further treatment at 5 years. It also preserves urinary continence in up to 98% and erectile function in about 78–85% of men. Some patients may need retreatment, and HIFU may be less effective for larger or hard-to-reach tumors.
4. Irreversible Electroporation (IRE)
IRE uses short bursts of electric current to create tiny holes in cancer cell membranes, leading to cell death. Unlike thermal therapies, IRE avoids heating and may better preserve surrounding tissues. Studies show up to 89% of men avoid further treatment for at least a year, and most maintain good urinary and sexual function, though mild changes in ejaculation can occur. IRE is well suited for tumors near sensitive areas, such as nerves or the urethra.
5. Radiofrequency Ablation (RFA)
RFA delivers electrical energy to create heat that kills cancer cells. It’s guided by imaging and targets MRI-visible tumors. In small studies, 80–90% of men had no cancer in the treated area 6 months after RFA. Side effects are typically mild, and most men retain urinary and sexual function. However, follow-up biopsies remain essential, as imaging alone may miss residual cancer.
6. Transurethral Ultrasound Ablation (TULSA)
TULSA delivers controlled ultrasound energy through a probe inserted into the urethra, guided by MRI in real-time. It can treat the whole prostate or just part of it. In recent studies, over 95% of men kept urinary continence, and most preserved sexual function. Cancer control is promising, with only a small number needing further treatment. TULSA is minimally invasive, done under anesthesia, and allows for precise targeting with fewer side effects than traditional treatments.
7. Vascular Targeted Photodynamic Therapy (VTP)
VTP is a light-activated treatment that uses a photosensitizing drug and a laser to kill cancer cells by generating reactive oxygen. It is the first focal therapy to show benefit in a randomized trial. In the PCM301 trial, men who received VTP had a 76% chance of avoiding radical treatment after 4 years, compared to 47% on active surveillance. Cancer control was good, and side effects were minimal. This makes VTP a promising option for men with low-risk prostate cancer.
A Quick Comparison of Focal Therapy Options
| Focal Therapy | Mechanism | FDA Approval | Pros | Cons | Insurance Coverage |
| Cryotherapy (Cryoablation) | Freezing probes create ice to kill tissue | Yes (for prostate cancer) | Minimally invasive, effective for small lesions, repeatable | Risk of erectile dysfunction, not ideal for large prostates | Covered by most insurance |
| Focal Laser Ablation (FLA) | Laser fiber heats and ablates cancerous tissue | For soft tissue/ not specifically for prostate carcinoma | Precise targeting, real-time imaging, low risk of complications | Limited long-term data, highly operator-dependent | Rarely covered |
| High-Intensity Focused Ultrasound (HIFU) | Ultrasound waves heat and destroy cancer cells | Yes (general prostate tissue ablation, not cancer-specific) | Non-invasive, preserves continence and sexual function, outpatient | May require retreatment, limited availability, cost | Not covered as primary treatment |
| Irreversible Electroporation (IRE) | Electric pulses create pores in cell membranes causing cell death | Approved for prostate tissue | Non-thermal, spares nearby structures, good functional outcomes | Requires anesthesia, lacks long-term oncologic data | Not covered |
| Radiofrequency Ablation (RFA) | Electric current heats tissue via radiofrequency energy | Investigational | Minimally invasive, good functional outcomes in early trials | Limited clinical data, not widely available | Rarely covered |
| Transurethral Ultrasound Ablation (TULSA) | MRI-guided ultrasound energy ablates tissue via a transurethral probe | Approved for BPH, prostate cancer use investigational | Real-time MRI guidance, customizable ablation, minimal side effects | Requires MRI equipment, currently limited to trials or select centers | Covered by original Medicare |
| Vascular-Targeted Photodynamic Therapy (VTP) | Light-activated drug generates reactive oxygen to destroy tumor | Approved in Europe, investigational in US | Targeted, preserves healthy tissue, evidence from randomized trials | Photosensitivity, limited access, still under study | Not commonly covered |
| Water Vapor Ablation | Heated water vapor delivered via urethra to thermally ablate cancer | Investigational – under evaluation in VAPOR 2 trial | Minimally invasive, preserves urinary/sexual function, under evaluation | Still investigational, long-term outcomes not yet known | Not yet covered (in clinical trials) |
Cryoablation, IRE, and Microwave Ablation: A Closer Look
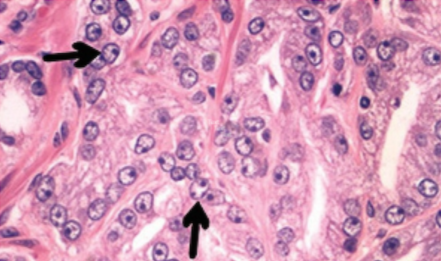
A recent systematic review published in Cancers (2024) analyzed 23 clinical studies on three minimally invasive focal therapies for localized prostate cancer: cryoablation, irreversible electroporation (IRE), and microwave ablation. These approaches aim to treat only the cancerous area of the prostate, minimizing damage to healthy tissue and preserving quality of life.
Cryoablation showed the most mature data, particularly effective in men with intermediate-risk cancer. In one study, 96% of men treated with whole-gland cryoablation were metastasis-free after 10 years. Hemigland cryoablation also showed strong results, with 82% cancer-free at 18 months and low rates of urinary or sexual side effects.
IRE demonstrated good cancer control and functional preservation. One large study showed 100% overall survival and 99% metastasis-free survival after focal treatment. Patients who received focal IRE were more likely to maintain erectile function than those treated with extended ablation.
Microwave ablation, while newer, showed high effectiveness in early studies. Over 90% of tumors were completely ablated within 6 months, with no significant changes in urinary or sexual function.
Although these findings are promising, larger and longer-term trials are still needed. For now, focal therapy is best considered for men with low- to intermediate-risk prostate cancer and should be pursued within clinical trials.
FAQs: Exploring Prostate Focal Therapy Options
Could TULSA be the Right Treatment for My Prostate Cancer?
If you’ve been diagnosed with localized prostate cancer and are looking for a treatment that preserves your quality of life, TULSA (Transurethral Ultrasound Ablation) might be an option to consider. This MRI-guided procedure uses a robotic ultrasound device inserted through the urethra to precisely heat and destroy cancerous prostate tissue—without the need for surgery or radiation. It can treat the whole prostate or just part of it.
A recent study by Lucas Engelage and Dr. Rolf Muschter, published in the Journal of Endourology (2025), followed 300 men who received TULSA for prostate cancer. Most had low- to intermediate-risk cancer and were between the ages of 60 and 73. After treatment, 96% of men kept full urinary control, and most maintained their erectile function. Side effects were generally mild and short-term, with no serious complications involving the bowel.
Cancer control was also promising. Only 14 men needed additional treatment, and many were able to continue with regular monitoring. These results suggest that TULSA can effectively treat prostate cancer while helping men avoid the long-term side effects of traditional treatments.
Am I a Good Candidate for Focal Therapy?
According to a recent review led by Dr. Alireza Ghoreifi (Prostate Cancer and Prostatic Diseases, 2024), the best candidates for FT are men with intermediate-risk, localized prostate cancer, especially when the cancer is found in just one area (unifocal). A multiparametric MRI (mpMRI) followed by targeted and systematic biopsy is essential before considering treatment.
- Most experts agree FT is appropriate for men with a Gleason score of 3+4 or 4+3, a PSA level under 10 ng/mL, and a tumor smaller than 1.5 to 3 mL seen on imaging. Having a prostate larger than 50 mL or erectile dysfunction doesn’t automatically rule you out, but may require extra planning.
- FT isn’t typically recommended for men with advanced or widespread disease, or for those with aggressive genetic markers like BRCA1/2 mutations. And since FT doesn’t treat the whole prostate, close follow-up with MRI and biopsy is crucial after treatment.
- Dr. Ardalan Ahmad and colleagues, in an article published by the American Urological Association, explain that the best candidates for focal therapy (FT) are men with intermediate-risk prostate cancer specifically Grade Group 2 or 3 (Gleason 3+4 or 4+3), PSA under 20 ng/mL, and cancer confined to the prostate.
- The tumor should be clearly visible on MRI, confirmed by targeted biopsy, and located in a single area that allows for safe treatment margins. FT isn’t ideal for high-risk or very low-risk cases.
- Age, prostate size, or erectile function don’t automatically exclude you. In fact, many men choose FT to help preserve urinary and sexual function. However, regular follow-up with MRI and biopsy is essential after treatment.
These two articles help guide doctors and patients in selecting the right candidates for focal therapy, but also highlight the need for more long-term data and ongoing research.

Could Focal Therapy be an Option for my Grade Group 3 Prostate Cancer?
In a recent review published in Current Urology Reports (2024) by Dr. Lee Pressler and colleagues, researchers looked at the safety and outcomes of FT specifically for men with GG3 prostate cancer. They found that while the risk of cancer returning in the treated area was somewhat higher than in lower-risk patients, the overall survival rates remained very high up to 96.6% at 8 years in some studies using high-intensity focused ultrasound (HIFU). Other techniques like cryotherapy and irreversible electroporation (IRE) also showed promising results in small studies, with many men avoiding whole-gland treatment and keeping their urinary continence and sexual function.
The authors emphasized that FT may be a good option for men with low-volume, localized GG3 cancer, especially when followed by close monitoring with MRI and biopsy. While not yet the standard treatment, FT offers hope for men who want to treat their cancer while maintaining a good quality of life.
Although these findings are promising, larger and longer-term trials are still needed. For now, focal therapy is best considered for men with low- to intermediate-risk prostate cancer and should be pursued within clinical trials.
Conclusion
Prostate focal therapy offers a targeted, less invasive option for treating prostate cancer with fewer side effects. By understanding your choices, you can make informed decisions that align with your health goals and lifestyle.
References
1. Ahmad AE, Yee C-H, Wysock JS, Ward JF. Focal therapy: defining candidates for partial gland prostate ablation: a critical challenge for focal therapy. AUANews. Published June 9, 2023. Accessed March 28, 2025. https://auanews.net/issues/articles/2023/june-2023/focal-therapy-defining-candidates-for-partial-gland-prostate-ablation-a-critical-challenge-for-focal-therapy
2. Allaway MJ, et al. Focal therapy for localized prostate cancer. AUA Update Series. 2020; Lesson 16. American Urological Association.
3. Engelage L, Muschter R. Transurethral ultrasound ablation for treatment of localised prostate cancer and benign prostatic hyperplasia (BPH). J Endourol. 2025;39(S1). doi:10.1089/end.2024.0301
4. Faiella E, Santucci D, D’Amone G, et al. Focal minimally invasive treatment in localized prostate cancer: comprehensive review of different possible strategies. Cancers (Basel). 2024;16(4):765. doi:10.3390/cancers16040765. PMID:38398156; PMCID:PMC10887212.
5. Ghoreifi A, Gomella L, Hu JC, et al. Identifying the best candidate for focal therapy: a comprehensive review. Prostate Cancer Prostatic Dis. Published online 2024. doi:10.1038/s41391-024-00907-y
6. Pressler L, Pressler M. Focal therapy in grade group 3 prostate cancer. Curr Urol Rep. 2024;25(11):271-275. doi:10.1007/s11934-024-01211-x. Epub 2024 Jul 2. PMID:38954356; PMCID:PMC11366723.
About The Authors

Teresa C. Gallagher, Ph.D., MPH is the CEO and Co-Founder of Sparrow Search, a digital health company reimagining clinical trial recruitment to make it more accessible, inclusive, and patient-centered. Prior to launching Sparrow Search, Dr. Gallagher conducted research on healthcare access at the Yale School of Medicine, Stanford University School of Medicine, and U.C.L.A. School of Medicine. She also served as a Professor of Community Health at the University of Illinois at Urbana-Champaign, where her work focused on health services utilization.

Martina Ambardjieva, M.D. Dr. Martina Ambardjieva is a urologist, researcher, and teaching assistant at the Medical Faculty of the University Ss. Cyril and Methodius in Skopje, North Macedonia. She is currently a Ph.D. candidate in clinical medicine, with research focused on urological oncology and the development of biomarkers in bladder cancer. Her clinical interests include cancer care and men’s health, with a strong dedication to education, early detection, and evidence-based practice. Dr. Ambardjieva also serves as the representative for international collaboration of the Macedonian Urological Association and actively contributes to scientific events across Europe.
About Sparrow Search

Sparrow Search simplifies clinical trial recruitment by helping patients quickly and privately discover studies that match their clinical history and preferences no physician referral needed. Built for both patients and pharmaceutical partners, Sparrow speeds up enrollment and helps bring new treatments to market faster. Learn more at SparrowSearch.Health.
Related Articles
Prostate Cancer Myths, Misconceptions, and the Urgent Need for Research and Reform
The Benefits of Joining a Prostate Cancer Support Group
Why Many Men with Metastatic Prostate Cancer Miss Out on Life-Extending Treatments



