By Teresa C. Gallagher, Ph.D., MPH. and Martina Ambardjieva, M.D.

Prostate cancer is the most common cancer in men after skin cancer, with about 1 in 8 men diagnosed during their lifetime, the same risk women face with breast cancer. Yet awareness, funding, and early screening practices remain strikingly low by comparison. On a global scale, rising life expectancy and aging populations are fueling what experts warn is a coming “prostate cancer tsunami.” As diagnoses climb each year, so too does the urgency for improved education, smarter screening strategies, awareness of clinical trials, and stronger investment in research. Understanding your risk is the first step, because prostate cancer is not just a disease of the old, and it’s certainly not a disease to ignore.
Prostate cancer recently returned to the public spotlight following U.S. President Joe Biden’s disclosure of his own diagnosis and treatment for prostate carcinoma. His case has raised important questions about PSA screening, the timing of diagnosis, and the biological behavior of prostate cancer. In particular, it has reignited discussion around what it really means for a prostate cancer to be “aggressive” a term that can refer to how quickly the cancer grows, its likelihood of spreading, and the potential need for urgent treatment. While many prostate cancers are slow-growing and may never cause harm, aggressive forms can be life-threatening if not detected and managed early.
Prostate Cancer Myths and Misperceptions
Despite being one of the most commonly diagnosed cancers in men, prostate cancer is often misunderstood, with many long-standing prostate cancer myths still influencing public perception. Misinformation or outdated assumptions can lead to delayed diagnosis, missed treatment opportunities, or unnecessary anxiety. In the following section, we address several widespread beliefs about prostate cancer and provide up-to-date, evidence-based explanations. Our aim is to support informed decision-making by helping patients, families, and caregivers better understand the realities of this complex disease.
Myth 1. PSA Testing Diagnoses Prostate Cancer
PSA testing is only one part of prostate cancer screening. A proper evaluation always includes a digital rectal examination (DRE), which can detect abnormalities even when PSA appears “normal.”
Additionally, PSA interpretation isn’t based solely on the absolute number. Parameters like PSA doubling time, PSA velocity, free PSA percentage, and PSA density are all critical. So, what is a “normal” PSA? That depends on the individual and their clinical context age, prostate volume, and other factors must be considered. This is precisely why PSA should always be interpreted by a urologist rather than in isolation.
It’s also important to understand the limitations of PSA testing. While helpful, it’s not perfect. According to the U.S. Preventive Services Task Force, PSA testing has a sensitivity of about 21% to 51% and a specificity of 91% for detecting prostate cancer. Sensitivity refers to the test’s ability to correctly identify individuals who have the disease, so lower sensitivity means some cancers, including aggressive ones, may be missed. Specificity, on the other hand, measures how well the test identifies those who do not have the disease, so higher specificity reduces the chance of false positives.
There are rare exceptions aggressive cancers in patients with low PSA levels, but these are not the rule. That’s why individualized risk assessment and expert interpretation are essential. The sensitivity and specificity of the PSA test for prostate cancer detection can vary depending on the PSA level thresholds used. For instance, a systematic review and meta-analysis found that for PSA levels between 4–10 ng/mL, the sensitivity is approximately 93.1%, while the specificity is around 29.3% . This indicates that while the test is quite sensitive in this range, its specificity is relatively low, leading to a higher rate of false positives.
It’s important to note that these figures can differ based on the population studied and the methodologies employed. Therefore, PSA testing should be interpreted in the context of individual patient factors and in conjunction with other diagnostic tools.
Myth 2. PSA Testing Should Not Be Done After Age 70
When it comes to prostate cancer screening, especially with PSA testing, major medical organizations emphasize individualized decision-making. The USPSTF recommends that men aged 55 to 69 make a personal decision about PSA-based screening after discussing the potential benefits and risks with their clinician, while it advises against routine PSA screening in men aged 70 and older.
Similarly, the American Urological Association (AUA) advises that clinicians offer regular screening every 2 to 4 years for men aged 50 to 69 (Strong Recommendation; Grade A Evidence), but also emphasizes that re-screening intervals and decisions to discontinue testing should be personalized based on patient preference, age, risk, PSA levels, life expectancy, and general health, all guided by shared decision-making.
The National Comprehensive Cancer Network (NCCN) also supports a risk-based, shared decision-making approach, recommending that average-risk men begin discussions about PSA testing at age 50, high-risk men (e.g., African American men or those with a family history) at age 45, and very high-risk individuals (e.g., BRCA mutation carriers) as early as age 40. The NCCN advises tailoring follow-up based on initial PSA levels and discourages screening in men with a life expectancy under 10 years or those over age 75, unless clinically appropriate.
Table 1. Clinical practice guidelines for PSA Testing
| Organization | Start Age | Routine Screening Age | Frequency & Notes |
| United States Preventive Services Task Force (USPSTF1) | 55 (average risk) | 55–69 (shared decision) | Discourage over 70 |
| American Urological Association (AUA) | 50 (average risk) Individualized for high-risk | 50–69 (shared decision) | Every 2–4 years |
| National Comprehensive Cancer Network (NCCN) | 50 (average) 45 (high risk) 40 (very high risk) | Risk-based, typically 50–75 | Tailored to PSA & risk Avoid if life expectancy <10 yrs or age >75 |
1These recommendations were published in 2018 and are currently under review, with an updated version anticipated in 2025.
Myth 3. Prostate Cancer Is a Disease of Old Men
Prostate cancer is often called a disease of old men, and statistically, that’s partly true. The median age at diagnosis is around 69, meaning half of all cases occur before that age, and half after. But here’s the nuance: the first half of cases happens across a broad age range, roughly from 40 to 69, almost 30 years. The other half occurs mostly between 69 and 80, a much shorter span and within a much smaller population group.
So, although the same number of cases are split across these two age bands, the incidence rate in older men is significantly higher. In other words, prostate cancer is more frequent in older men, not because younger men are unaffected, but because the same number of cases are concentrated in fewer people.
It’s true that risk rises with age, but let’s not forget that many men are diagnosed in their 40s, 50s, and 60s. Dismissing prostate cancer as a disease only of the elderly risks delaying early diagnosis in younger patients who may otherwise benefit from timely intervention.
Myth 4. Prostate Cancer Is An “Indolent” or “Innocent” Disease.
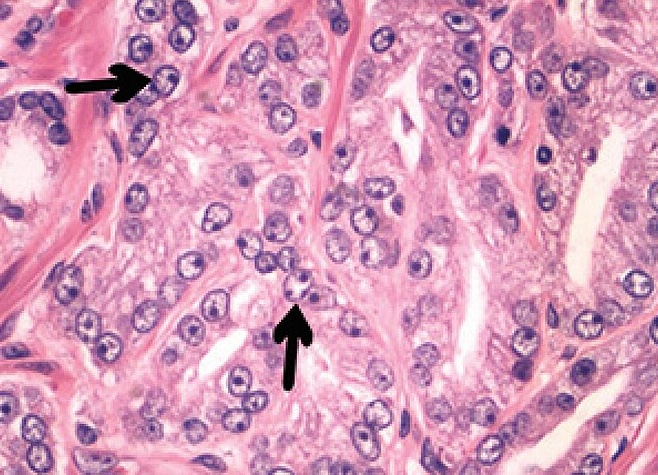
Calling prostate cancer indolent means that it tends to grow slowly, not that it’s harmless. But this can be misleading. Many hear ‘indolent’ and think innocent or not dangerous, which isn’t accurate. While it’s true that some types of prostate cancer progress slowly and may not require immediate treatment, others are aggressive from the start.
The key is that we can’t always predict at diagnosis which cancers will remain slow-growing and which will become life-threatening. That’s why regular monitoring, accurate risk stratification, and personalized treatment plans are so important. ‘Slow growing’ doesn’t mean “safe to ignore.”
Myth 5. You Are More Likely to “Die With” Than “Die From” Prostate Cancer.
It’s often said you’re more likely to die with prostate cancer than from it, but that overlooks the real danger. In the U.S., a man dies from prostate cancer every 15 minutes. In 2025, over 35,000 men in the U.S. alone are expected to die from prostate cancer. Globally, the number exceeds 375,000 annually (according to Globocan, Figure 1).
While many cases are slow-growing, aggressive forms exist and can be deadly if not caught early. ‘Indolent’ doesn’t mean harmless; early detection still saves lives.

Myth 6. “Aggressive” Prostate Cancer is A Death Sentence
A diagnosis of aggressive prostate cancer, such as Gleason score 9, is serious but not necessarily a death sentence. Advancements in treatment have significantly improved outcomes, allowing many men to live 10 years or more post-diagnosis. The key lies in early detection, personalized therapy, and access to innovative treatments.
As of May 2025, ClinicalTrials.gov lists over 1,400 active clinical trials related to prostate cancer, encompassing various stages and treatment modalities. These trials explore therapies ranging from hormone treatments and chemotherapy to cutting-edge approaches like radiopharmaceuticals, immunotherapies, and targeted therapies.
Here are some of the most promising therapies currently under investigation or recently approved for metastatic prostate cancer
- PSMA-Targeted Radioligand Therapy (e.g., Lu-177 vipivotide tetraxetan / Pluvicto)
This therapy delivers radioactive particles directly to prostate cancer cells expressing PSMA, minimizing damage to healthy tissue. Clinical trials have demonstrated improved survival rates and delayed disease progression. - JANX007 (Janux Therapeutics)
An experimental T-cell engager targeting PSMA, JANX007 has shown remarkable results in early trials, with significant PSA reductions in heavily pretreated patients. Its dual mechanism enhances immune response while limiting toxicity. (You can learn more about participating in a JANX007 clinical trial here.) - Niraparib + Abiraterone Acetate (Akeega)
This combination therapy targets DNA repair pathways and androgen production, showing efficacy in patients with BRCA mutations. Approved in the U.S. and EU, it’s a promising option for certain metastatic castration-resistant prostate cancer (mCRPC) patients. - Relugolix (Orgovyx)
An oral hormone therapy that suppresses testosterone production, Relugolix offers a convenient alternative to injections with fewer cardiovascular risks. It’s approved for advanced prostate cancer and is being studied in combination therapies. - Gridegalutamide (BMS-986365) & Luxdegalutamide (ARV-766)
These investigational drugs belong to a class called PROTACs, designed to degrade androgen receptors and overcome resistance to traditional therapies. Early studies indicate potential benefits for patients with treatment-resistant mCRPC. - Talzenna + Xtandi (Pfizer)
This combination has shown improved overall survival in late-stage studies for mCRPC patients, regardless of genetic mutations, and is under review for broader use.
Myth 7. Treatment Cures Prostate Cancer
While treatments for prostate cancer, such as radical prostatectomy, radiation therapy, and androgen deprivation therapy, can be highly effective, the term “cure” should be used cautiously. Although many men with localized prostate cancer achieve long-term remission, especially with low-risk disease, recurrence remains a significant concern, particularly in patients with high-risk or aggressive subtypes such as Gleason 8–10 tumors. Biochemical recurrence, marked by a rising PSA after treatment, may occur even years later and can sometimes signal a more aggressive and treatment-resistant disease.
Prostate cancer is biologically heterogeneous and often unpredictable, with some initially indolent cancers progressing rapidly or responding poorly to standard therapies. Moreover, life-altering side effects, including urinary incontinence, erectile dysfunction, bowel dysfunction, metabolic changes, and mood disturbances, are common across treatment modalities and can significantly impact quality of life.
Consequently, long-term management and careful shared decision-making are essential. Emerging genomic tools and biomarkers are helping stratify risk and personalize treatment, but no single therapy guarantees a cure across all patient populations.
Note: It is highly recommended that patients join a prostate cancer support group to enhance treatment success and emotional well-being.
Myth 8. The Pharmaceutical Industry Pays For All Prostate Cancer Research. We Do Not Need Government or University Funding.
Despite a growing “prostate cancer tsunami” as populations age, the U.S. President’s budget proposal would slash NIH funding by $18 billion, a nearly 40% cut, threatening hundreds of critical cancer research projects.
While universities and other organizations fund the majority of ongoing clinical trials, and the pharmaceutical industry contributes to some, the NIH plays a uniquely vital role in supporting early-phase, prevention, and disparity-focused studies areas often overlooked by other funders.
As of now, dozens of prostate cancer trials remain NIH-funded, but that number may drop fast without urgent action.
We must protect funding for prostate cancer research. Lives depend on it.
- Search NIH-funded prostate cancer trials
- Support Prostate Cancer research – Prostate Cancer Foundation
- Search all prostate cancer clinical trials- Sparrow Search
Conclusion
Understanding prostate cancer myths is essential to ensure timely diagnosis and effective treatment. Correcting these myths can help save lives through early detection.
References:
- Okwor, C. J., Nnakenyi, I. D., Agbo, E. O., et al. (2023). Sensitivity and specificity of prostate-specific antigen and its surrogates towards the detection of prostate cancer in sub-Saharan Africa: A systematic review with meta-analysis. African Journal of Urology, 29(41).
https://doi.org/10.1186/s12301-023-00372-4 - U.S. Preventive Services Task Force. (n.d.). Prostate cancer: Screening. Retrieved May 2025, from https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/prostate-cancer-screening
- Wei, J. T., Barocas, D., Carlsson, S., Coakley, F., Eggener, S., Etzioni, R., Fine, S. W., Han, M., Kim, S. K., Kirkby, E., Konety, B. R., Miner, M., Moses, K., Nissenberg, M. G., Pinto, P. A., Salami, S. S., Souter, L., Thompson, I. M., & Lin, D. W. (2023). Early detection of prostate cancer: AUA/SUO guideline part I: Prostate cancer screening. The Journal of Urology, 210(1), 46–53.
https://doi.org/10.1097/JU.0000000000003491 - National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Prostate Cancer Early Detection. Version 1.2024 [Internet]. NCCN.org. Available from: https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1460
- ZERO Prostate Cancer. Prostate Cancer Facts and Statistics. https://zerocancer.org/about-prostate-cancer/facts-statistic
- Ferlay, J., Ervik, M., Lam, F., Laversanne, M., Colombet, M., Mery, L., Piñeros, M., Znaor, A., Soerjomataram, I., & Bray, F. (2024). Prostate cancer fact sheet. Global Cancer Observatory: Cancer Today, International Agency for Research on Cancer. https://gco.iarc.who.int/media/globocan/factsheets/cancers/27-prostate-fact-sheet.pdf
- American Association for Cancer Research. (2025, May 6). AACR calls on Congress to summarily reject the President’s FY2026 budget proposal for NIH. https://www.aacr.org/about-the-aacr/newsroom/news-releases/aacr-calls-on-congress-to-summarily-reject-the-presidentsfy2026-budget-proposal-for-nih/
- Fierce Biotech. Trump’s proposed cuts to federal cancer research ‘threaten all we have gained’: ASCO CEO. https://www.fiercebiotech.com/research/trumps-proposed-cuts-cancer-research-threaten-all-we-have-gained-asco-ceo
About the Authors

Teresa C. Gallagher, Ph.D., MPH is the CEO and Co-Founder of Sparrow Search, a digital health company reimagining clinical trial recruitment to make it more accessible, inclusive, and patient-centered. Prior to launching Sparrow Search, Dr. Gallagher conducted research on healthcare access at the Yale School of Medicine, Stanford University School of Medicine, and U.C.L.A. School of Medicine. She also served as a Professor of Community Health at the University of Illinois at Urbana-Champaign, where her work focused on health services utilization.

Martina Ambardjieva, M.D. Dr. Martina Ambardjieva is a urologist, researcher, and teaching assistant at the Medical Faculty of the University Ss. Cyril and Methodius in Skopje, North Macedonia. She is currently a Ph.D. candidate in clinical medicine, with research focused on urological oncology and the development of biomarkers in bladder cancer. Her clinical interests include cancer care and men’s health, with a strong dedication to education, early detection, and evidence-based practice. Dr. Ambardjieva also serves as the representative for international collaboration of the Macedonian Urological Association and actively contributes to scientific events across Europe.
About Sparrow Search
Sparrow Search simplifies clinical trial recruitment by helping patients quickly and privately discover studies that match their clinical history and preferences no physician referral needed. Built for both patients and pharmaceutical partners, Sparrow speeds up enrollment and helps bring new treatments to market faster. Learn more at SparrowSearch.Health.